NAD+ Precursor Stimulates the Production of Blood Cells
An international team of scientists discovered that dietary supplementation of nicotinamide riboside can maintain the balance within blood-making stem cells and speed up blood cell generation.
Blood, which makes up about 8 percent of an average person’s weight, plays a crucial role in delivering nutrients, carrying oxygen, transporting waste products and fighting pathogens. A rapid growth in abnormal blood cells that cannot carry out its duty leads to blood cancers that can be lethal, such as lymphoma and leukemia.
Blood cancer patients go through radiation or chemotherapy to get rid of the cancerous blood stem cells and replace them with new and healthy ones through stem cell transplantation. However, up to 25 percent of these cases don’t survive because the replenishment of blood cells is too slow. An international team of scientists found a way to speed up blood production by boosting the activity of blood-making stem cells with a vitamin B3 analog — nicotinamide riboside (NR).
A small pool of blood-making cells is responsible for the production of 1011 mature blood cells per day in a healthy adult. These blood-forming cells, called hematopoietic stem cells (HSC), found in the bone marrow, have unique properties: they can self-renew, differentiate into specialized cells, mobilize out of the bone marrow into the blood and induce self-destruction.
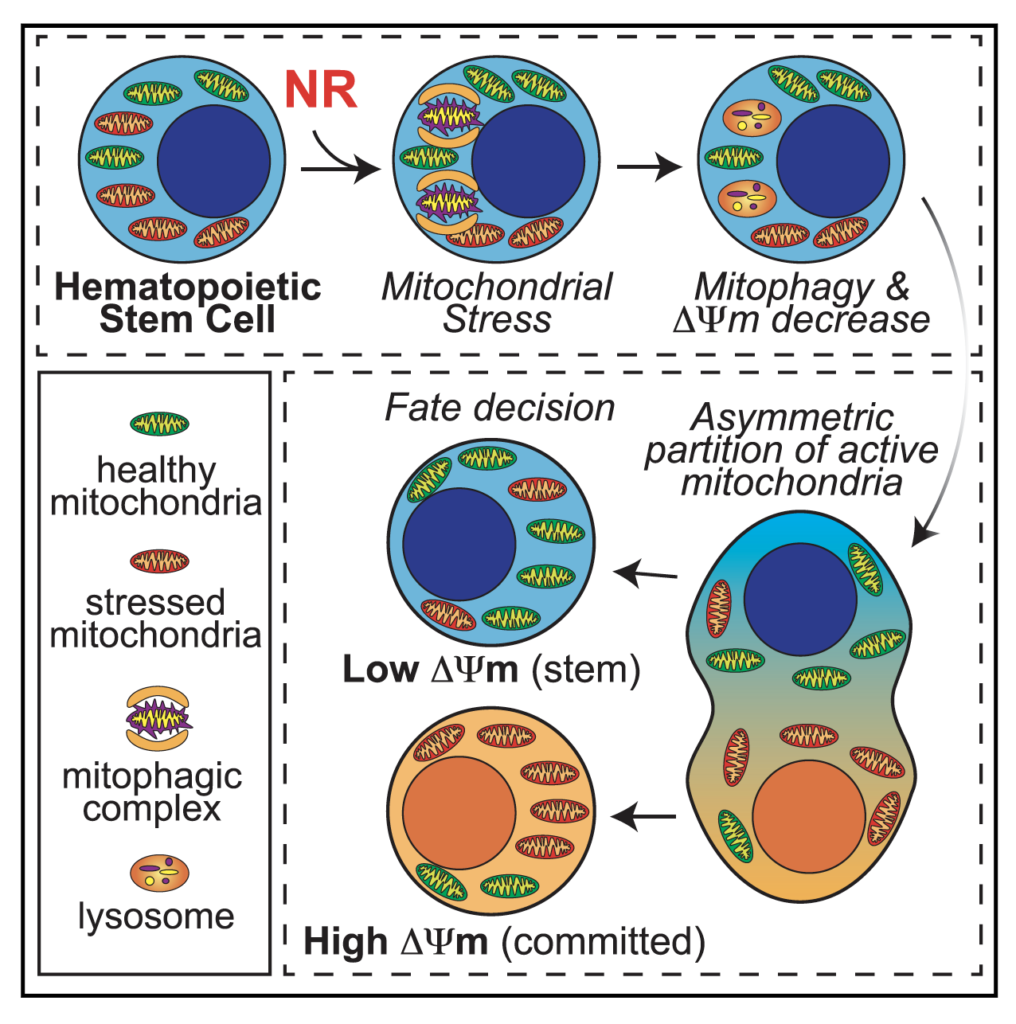
Although HSCs are powerful, reconstituting the entire blood-cell supply system can be an overwhelming job. The stress of producing blood cells for the body triggers the mitochondria, the powerplant of cells, to increase oxidative phosphorylation — the process of energy generation. But boosting the mitochondria activity comes at the cost of the stem cells aging prematurely.
NR Improves Blood Stem Cell Function
Previous studies showed that the vitamin B3 analog, NR, activates pathways that respond to mitochondrial stress in body tissues and muscle regeneration. When researchers introduced NR to human and mouse HSCs, the function of the stem cells improved and increased mitochondrial recycling, which the cells rid themselves of the stressed-out, damaged mitochondria for new, healthy ones.
Naveiras and colleagues describe the effects of vitamin B3 derivatives in blood formation, of which they find nicotinamide riboside (NR) to most potently increase blood progenitors. Treating purified mouse or human blood stem cells with NR improved their mitochondrial quality and reduced the toxicity of bone marrow transplantation in mice. (Vannini et al., 2019)
To test whether NR increases the survival of HSC transplantation, the team put mice through irradiation procedures to eliminate their blood cells and treated them with low-dose HSC transplantation. While none of the mice fed with a regular diet survived, NR-fed mice had an 80 percent chance of survival after the experiment, along with accelerated blood recovery. In immune-deficient mice, NR also increased the production of leukocytes, white blood cells.
“We expect nicotinamide riboside and other mitochondrial modulators to become a complementary approach for increasing stem cell fitness and accelerating blood production, either through dietary supplementation or pharmacological administration,” says senior author Olaia Naveiras of Ecole Polytechnique Fé dé rale de Lausanne (EPFL), Switzerland, in a statement.
This study is the first to demonstrate that NR, as a dietary supplement, can boost the function of the blood stem cells, unveiling NR’s potential to prevent blood-recovery failures. The researchers also noted that the NR and other molecules with similar functions, such as nicotinamide mononucleotide, might become a supportive treatment that expands beyond blood-cancer patients. It may also help patients with blood-related autoimmune disorders in the future.

