The Molecules SS-31 and NMN Synergistically Improve Aged Heart Function
Scientists treated old mice with the molecules SS-31 and NMN (nicotinamide mononucleotide) separately to improve different heart functions and when delivered together these molecules acted synergistically to recapitulate the function and metabolism of young hearts.
Cardiovascular disease is a major cause of death in older people, with greater mortality than all types of cancer in adults older than 75 years of age combined. When heart function declines with age, phases of the heartbeat get disrupted–specifically, when the heart fills with and pumps out blood. Due to the mortality rate from cardiovascular disease and the associated health costs, identifying therapeutic options to treat dysfunctional heartbeat and overall cardiac function remain a top priority for researchers.
Scientists from the University of Washington published a study in Aging Cell where they found that two therapeutic options SS-31 and nicotinamide mononucleotide (NMN) improved cardiac function in old mice to similar levels of young mice. When old mice were treated with each of these two drugs, the investigators saw that different aspects of cardiac function improved and that combining them facilitated a synergistic improvement in overall heart function. “These results may have strong clinical relevance and imply that synergistic treatment with the two drugs in combination may be more effective at treating age‐related heart dysfunction than either given alone,” said the investigators.
Previous research has indicated that SS-31, also known as elamipretide, reduces cellular stress, but the underlying mechanisms remain unclear. Indications show that SS-31 promotes the health of the cell’s powerhouse, the mitochondria, which contributes to these cellular benefits.
NMN boosts levels of a molecule called nicotinamide adenine dinucleotide (NAD+) that has essential roles in cellular energy production and health. NMN improves mitochondrial health by increasing levels of cellular NAD+ to enhance cellular energetic capacity. Evidence supporting this comes from scientific studies showing that NMN treatment improves signs of aging and age-related diseases in mice.
For these reasons, Whitson and colleagues tested the effects of these two mitochondrial-targeted drugs SS-31 and NMN on old mouse hearts. The investigators treated older animals with SS-31 and NMN both individually and in combination, and all treatments resulted in diminished age-related metabolic changes in cardiac function. They next measured the ratio of the metabolites phosphocreatine (PCr) and adenosine triphosphate (ATP) in the heart during experimentally-induced elevations in heart rate in these old mice. This measurement provides an assessment of how effectively the heart can respond to increased work by determining the degree to which the phosphates stored in PCr that provide energy for contraction are depleted from cardiomyocytes under increased demand for ATP.
The investigators found that treating old mice with either drug individually or in combination improved age-related changes in the ratio of metabolites PCr to ATP. The reversal of changes in this ratio with either treatment individually or in combination indicated a restored ability of the older hearts to handle a higher workload and heart rate.
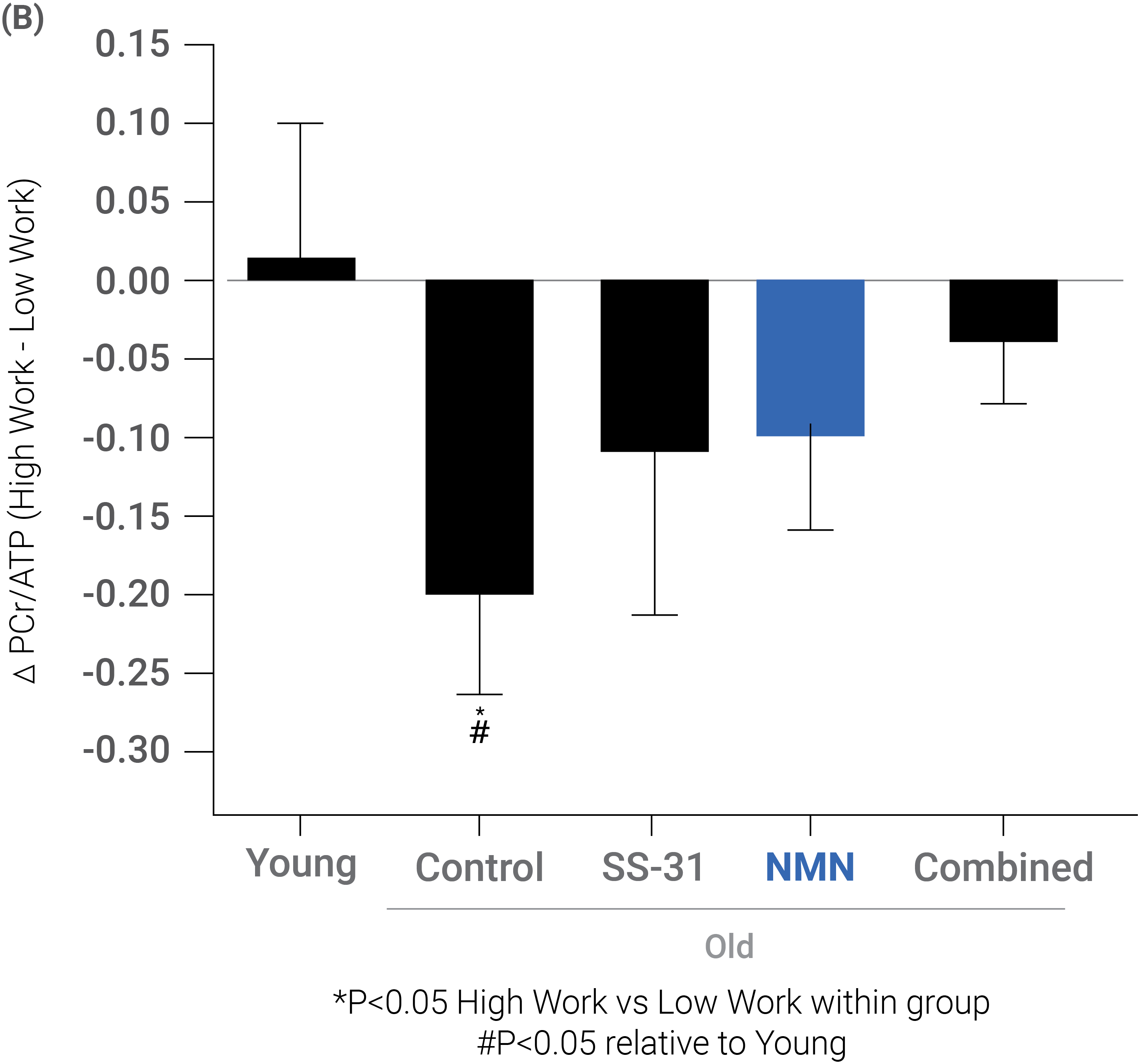
(Whitson et al., 2020 | Aging Cell) SS-31, NMN, or a combination of treatments restored the metabolic profile of heart in older mice. (B) Treatment with SS-31, NMN, or the combination of the two treatments improved the metabolism in older hearts toward that of younger mice as represented by the PCr/ATP ratio.
A Combination of SS-31 and NMN Additively Improves Heart Function
Interestingly, the investigators found that treating older mice with either SS-31 or NMN resulted in improvements in different aspects of cardiac function. Older mice treated with SS-31 showed significant rejuvenation to diastolic function, the period of the heartbeat where the heart’s chambers fill with blood. NMN treatment resulted in marked improvements in systolic function, the period of the heartbeat where the heart pumps blood throughout the body. Importantly, combined treatment with SS-31 and NMN improved both diastolic and systolic function.
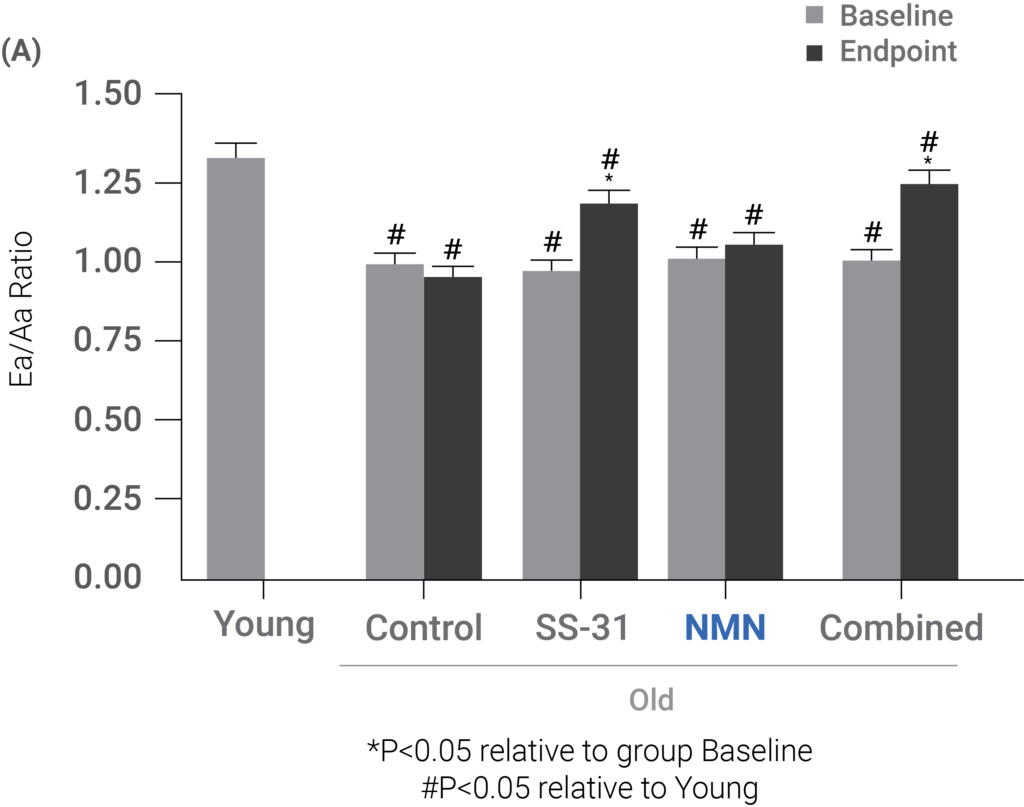
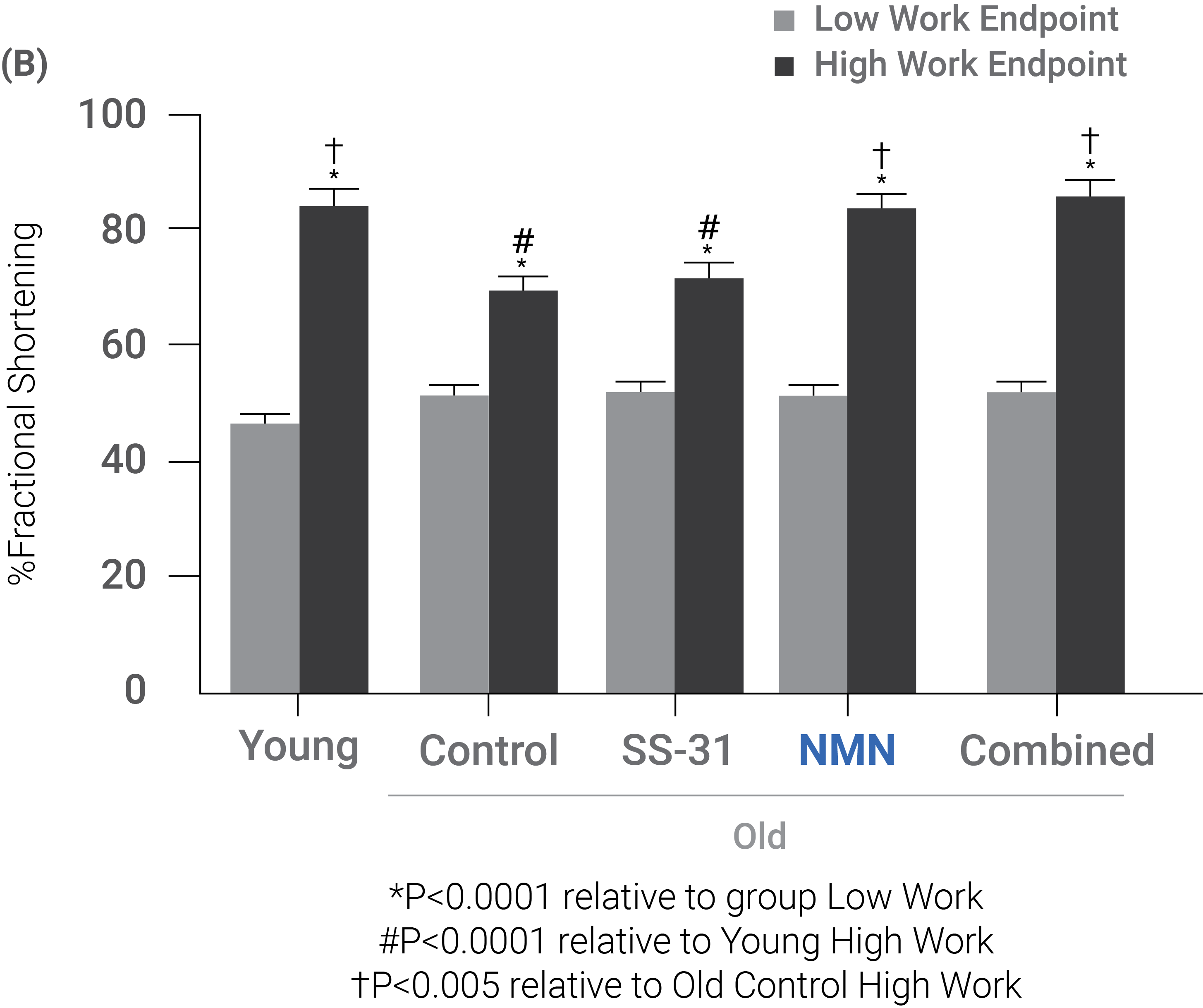
(Whitson et al., 2020 | Aging Cell) SS-31 improves the period of the heartbeat where the heart’s chambers fill with blood (i.e., diastolic function), NMN improves the period of the heartbeat where the heart pumps blood throughout the body (i.e., systolic function), and the combination improves both diastolic and systolic functions in older mice. (A) After treating old mice with SS-31, diastolic function, as represented by the Ea/Aa ratio, improved toward that seen in young mice. These improvements came with a combination of SS-31 and NMN, also. (B) After treating old mice with NMN, their systolic function, as represented by percent fractional shortening, in higher workload conditions improved to that seen in young mice. Similar results were observed with a combination of treatments.
“Since giving the drugs in combination conferred both diastolic and systolic improvements, but neither prevented nor further added to the individual improvements, the data imply that the drugs use two independent mechanisms to achieve these functional benefits,” stated the investigators in their study. On the one hand, NMN has a more acute effect than SS-31, with its effects disappearing after 10 days of treatment cessation. On the other hand, the effects of SS-31 persist for several weeks after cessation. These different timelines of effectiveness fit the proposal that NMN primarily works to boost NAD+ levels thereby quickly enhancing heart muscle energy supply, whereas SS-31 repairs mitochondrial efficiency and reduces cellular stress to facilitate remodeling of heart cells, which takes weeks.
The study demonstrates that the two drugs can be administered together to rejuvenate both diastolic and systolic functions. “By testing SS‐31 and NMN together in mice, we were able to provide new insight into the effects and mechanisms of each drug in the heart,” said the investigators in the study. According to the research team, the results imply that combinatorial treatment with the two drugs could be more effective than either on its own in treating age-related cardiac dysfunction. They conclude that using complementary drugs may provide a model to achieve optimal extensions of healthspan.

