How Treating Aging Itself Might Help Overcome COVID-19
Gerontologists who study the science of aging proposed that targeting aging-related pathologies can be a new strategy to fight the pandemic and the health and economic benefits will outlive COVID-19.
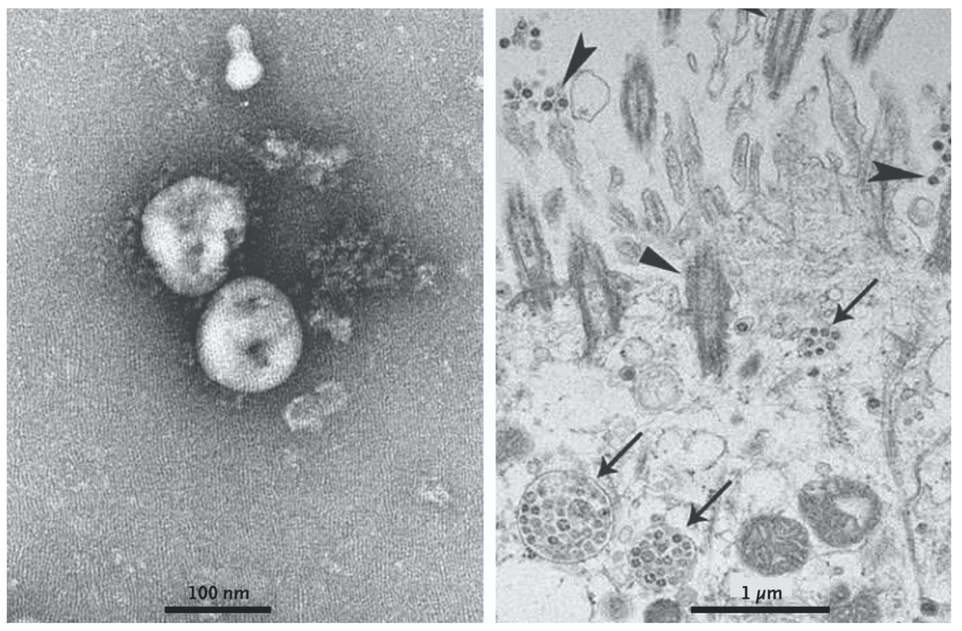
Spreading like wildfire in the cities, COVID-19 scorched the world with a pneumonia-like illness. Adults over 60, particularly those with underlying medical conditions, are more likely to have severe, even deadly, infections than other age groups. A new review paper published March 30 in the journal Aging proposed that targeting aging-related pathologies can be a new strategy to fight the pandemic.
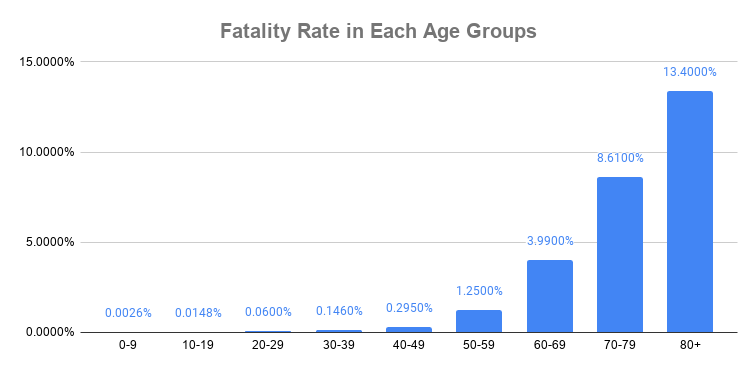
As statistics show that COVID-19 disproportionately infects older adults, the paper proposed that the disease is gerolavic — harmful to the old. An estimated 13.4% of patients 80 and older die from COVID-19, while 1.25% of those in their 50s and 0.06% of those in their 20s. Given the gerolavic nature of COVID-19, strategies targeting age-associated pathologies and immune dysfunction is a new angle to tackle the disease.
“On one hand, there is a declining immune response, so the elderly get sick much faster. But the second thing that gets them into trouble in the ICU and what they die from is an inflammation that happens in their lungs mainly,” says Nir Barzilai, the director of the Institute for Aging Research at Albert Einstein College of Medicine, who is not affiliated with the published paper.
Treating with NAD+ Boosters
Besides investigating vaccines and traditional antiviral therapies, the paper calls for investigating geroprotectors — compounds that target aging to promote healthspan and longevity. Commercially available medications such as the immunosuppressive drug, rapamycin, and the anti-diabetic medicine, metformin, both show potential as geroprotectors in early clinical trials. Other methods suggested include the widely available NAD boosters and caloric restrictions that showed anti-aging properties in animal studies.
Gerontologists that study the science of aging have agreed on eight hallmarks of aging, including immune dysfunction and inflammation, that are relevant to COVID-19. These hallmarks are interconnected, which means that therapies targeting on any one of them will affect the others.
“Aging is the one that drives the disease,” says Barzilai. The older one becomes, the higher the chances that one develops conditions such as cardiovascular diseases, diabetes, and neurodegeneration. “We cannot treat diseases individually anymore. What we need to do is to target the aging effect because only [by] targeting the aging effect, will everything [be affected].
“The virus SARS-CoV-2, which causes COVID-19, is genetically similar to the coronaviruses that caused respiratory illness SARS and MERS. Theoretically, treatments effective against SARS and MERS offer the most promising starting point for developing therapies against COVID-19. However, those epidemics quickly subsided, and the scale of the outbreak did not provide commercial benefits for pharmaceutical companies to develop effective drugs.
Simply put, the discovery efforts stopped.
“Pathogens can change,” says Sean Leng of Johns Hopkins University, in a webinar on COVID-19 and the impact on older adults. “Even the coronavirus family alone, we saw SARS, MERS, and now COVID-19. If we only go after the pathogens, we’re not going to get very far. That’s why we need to think of the geroscience approach.”
Recently, scientists identified 69 drugs that may be effective against COVID-19, which includes geroprotectors such as rapamycin and metformin. However, to Barzilai’s frustration, those drugs are not in the line for clinical trials against the disease.
As a scientist, Barzilai is careful and conservative. He believes that drugs should go through clinical trials. But when his 90-year-old father-in-law came to him and asked, “Can you protect me?” He gave his father-in-law metformin, an anti-diabetic drug currently under clinical trial for its potential to target aging, led by Barzilai.
“Am I doing the right thing?” Barzilai asked himself. “It’s a very hard ethical dilemma to have so much science, so much experience, such a good drug that is safe and is going nowhere when the disease is ramping [up in] the elderly. Not fair.”
Another recent study proposes starting clinical trials with low-dose rapamycin, an immunosuppressive drug that is also a geroprotector, to protect the elderly from the pandemic.
The new coronavirus has substantial effects on older adults. Targeting aging can increase the body’s resiliency to illness, decreasing the severity and lethality of the disease. Aging research not only yields insights that may help COVID-19 but is also a sustainable solution that will outlive the pandemic by helping to prevent or mitigate age-related diseases. The commercial benefits can also stimulate pharmaceutical companies to invest and develop geroprotector drugs.
In these desperate times, scientists around the world hunt for a safe and effective cure for COVID-19. Gerontologists believe they can help by tackling the root of disease — aging. “This science went from hope to promise, to realizing the promise,” says Barzilai. Prosecuted with caution, now is the time to enter clinical trials and find out.

