Study Shows NMN Alleviates Inflammation-Induced Lung Injury in Mice
Chinese scientists find that nicotinamide mononucleotide (NMN) reduces lung tissue damage while reducing inflammation and oxidative stress — cell damage caused by excessive reactive molecules.
Highlights:
- Mice injected with NMN are protected against lung tissue injury in response to damaging levels of inflammation.
- NMN reduces inflammatory protein levels in fluid from injured lungs.
- Protein markers of oxidative stress in response to injury are reduced by NMN.
Older individuals are particularly susceptible to sepsis — a life-threatening inflammatory reaction to infection, often starting in the lungs. Sepsis-induced lung injury leads to respiratory dysfunction, with a mortality rate of 30-40%. Thus, NMN, as a precursor of NAD+, an essential molecule capable of reducing inflammation, may provide a potential treatment option for sepsis-induced lung injury.
Researchers from the Changhai Hospital in China report in the Journal of Surgical Research that NMN alleviates inflammation-induced lung injury. To model sepsis and induce acute lung injury, Tian and colleagues injected mice with lipopolysaccharide (LPS). In these sepsis model mice, NMN was shown to reduce several pathological features of lung injury while reducing markers of inflammation and oxidative stress, suggesting that NMN could be used to treat sepsis-induced lung injury.
NMN Reduces Infection-Induced Lung Injury, Inflammation, and Oxidative Stress
LPS is a component of bacteria that induces inflammation and oxidative stress, both involved in the genesis of acute lung injury. To model sepsis-induced lung injury, Tian and colleagues exposed mice to LPS. The sepsis mice were then treated with 500 mg/kg of NMN via injection into the abdominal cavity. Next, the researchers euthanized the mice and removed their lungs for analysis.
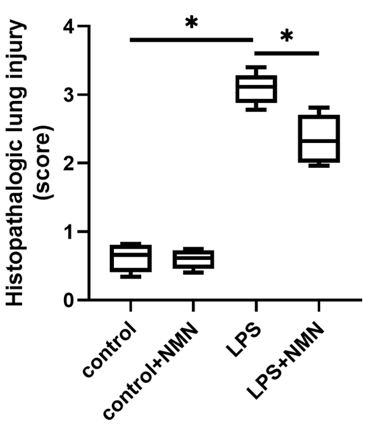
Lung damage was assessed by two independent pathologists (medical doctors). The pathologists scored lung injury based on factors like the structure of alveoli — the air sacs of the lungs — and inflammatory cell infiltration (inflammatory cells usually navigate to sites of damaged tissue). While the lung injury score increased in response to LPS, the score decreased with NMN treatment.
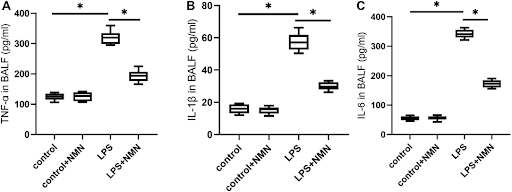
To assess lung inflammation, Tian and colleagues measured molecules called cytokines. Some of the most common cytokines associated with inflammation, TNF-α, IL-1β, and IL-6 were elevated in lung fluid from the sepsis model mice. However, NMN treatment reduced the protein levels of all three pro-inflammatory markers, suggesting NMN reduces lung infection-induced inflammation.
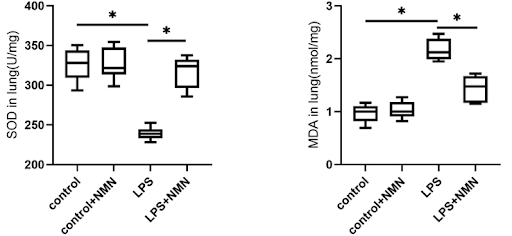
In response to aging, as well as injury, both inflammation and oxidative stress levels increase. One of the reasons our oxidative stress levels increase with aging is a decline in cellular antioxidants, such as superoxide dismutase (SOD). Tian and colleagues found that SOD was reduced in the lung tissue of sepsis mice. Additionally, a marker of oxidative stress called MDA was increased. However, NMN increased SOD and decreased MDA, suggesting that NMN reduces infection-induced oxidative stress.
Boosting NAD+ to Prevent Lung Aging
Tissue damage via injury has many similarities to tissue damage via aging, including increased inflammation and oxidative stress. Indeed, tissue damage, especially due to infection, is known to accelerate the aging process. In response to injury and aging, cells tend to die off, which is often related to dysregulated energy utilization. Since NAD+ is a central mediator of cellular energy metabolism, it may help alleviate tissue damage caused by aging and injury.
A previous study has shown that boosting NAD+ increases the lifespan of septic mice and increases lung energy levels. Additionally, sirtuins, which are dependent on NAD+, may reduce lung fibrosis — a symptom of aging and injury. Boosting NAD+ with NMN, inhibits COVID-19 lung infection. Furthermore, NMN reduces injury-induced senescence — cells associated with injury and aging — in the lungs. Overall, it seems that boosting NAD+ could be a promising antidote to lung injury and aging.
Model: C57BL/6J mice
Dosage: 500 mg/kg NMN intraperitoneally injected

