Researchers Discover The Natural Compound Berberine Could Treat Stroke Damage
Supplementing stroke-damaged mice with berberine decreases brain inflammation and improves neurological function, possibly via the gut.
Highlights:
- Treating a mouse model for intracerebral hemorrhage (ICH) – a stroke subtype– with berberine reduces brain inflammation (neuroinflammation) and enhances neurological function.
- Abolishing healthy gut microbiota – trillions of diverse microorganisms key to gut health – in ICH mice eliminates berberine’s neuroprotective effects.
Nearly 20% of all strokes are caused by an intracerebral hemorrhage (ICH), a blood clot in the brain that often occurs in aged individuals and those with high blood pressure (hypertension). ICH inevitably triggers neuroinflammation, leading to brain damage and, ultimately, neurological dysfunction. With this in mind, researchers have focused on identifying interventions capable of alleviating brain inflammation following ICH injury, particularly through a known modulator of brain homeostasis – the gut microbiome.
Published in the journal Aging, researchers from Zhejiang University in China explored the neuroprotective effects of berberine, a natural and powerful anti-inflammatory compound widely utilized in traditional Chinese medicine. Chen and colleagues found that treating ICH mice with berberine significantly decreased brain inflammation and boosted neurological function. Additionally, the investigators showed that berberine treatment improved gut health by decreasing gut permeability, a known driver of neuroinflammation. Notably, berberine’s neuroprotective effects were reversed after eliminating beneficial gut microbiota in ICH mice, highlighting the relationship between berberine and the microbiome.
Berberine Limits Brain Inflammation and Neurological Dysfunction
Microglia cells — the brain’s resident immune cells — play a central role in mediating neuroinflammation, as their activation controls whether pro-inflammatory or anti-inflammatory molecules get secreted into the brain. Accordingly, activated microglia exist in one of two states: pro-inflammatory (M1) or anti-inflammatory (M2). Following ICH injury, there’s an increase in M1 microglia, which promote neuroinflammation and neurological dysfunction. Given berberine’s potent anti-inflammatory properties, Chen and colleagues wanted to see if supplementation could rescue neuroinflammation by modulating M1 and M2 microglia.
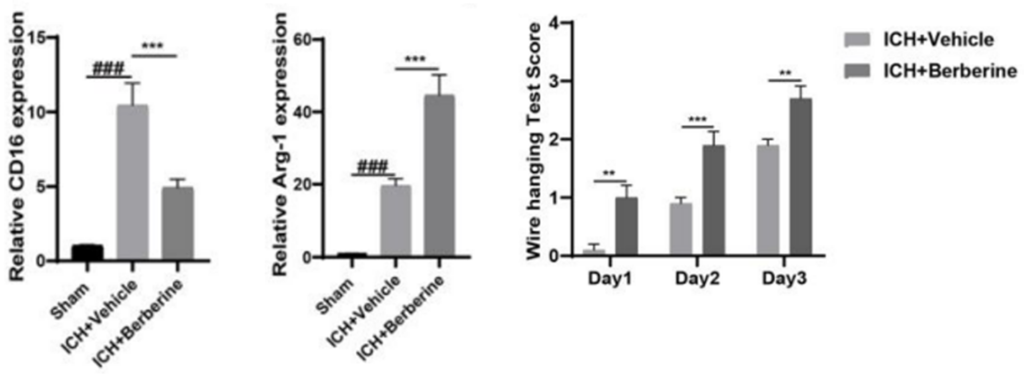
The investigators found that berberine treatment in mice attenuated the increases in M1 microglia following ICH injury and elevated the levels of activated M2 microglia. Furthermore, the results showed that supplementation led to significant decreases in pro-inflammatory molecules (IL-1β, TNF-α, CD206) and increases in anti-inflammatory molecules (Arg-1, CD16), confirming that berberine ameliorates ICH-induced neuroinflammation by regulating M1 and M2 microglia.
The research team then conducted an array of neurobehavioral tests to determine whether berberine’s effects on neuroinflammation contribute to enhanced neurological function. Berberine’s neuroprotective effects were most notably seen in the wire hanging test, where mice were evaluated on their ability to hold onto the top of a hanging wire and safely climb down. Higher scores indicated improved motor coordination, and the results demonstrated that berberine-treated mice displayed much higher scores than untreated ICH mice, indicating greater motor function. Overall, the findings suggest that berberine protects against neurological dysfunction in ICH mice by modulating neuroinflammation.
Berberine Depends on The Microbiome
Another primary contributing factor to brain health following an injury like ICH is the gut, whose permeability greatly influences the abundance of toxic molecules and neuroinflammation. Studies have shown that berberine interacts with the microbiome, so Chen and colleagues sought to determine if berberine’s effects on inflammation were linked to microbiome changes, specifically gut permeability. The research team showed that berberine-treated mice with reduced brain inflammation exhibited less permeable guts than untreated ICH mice, highlighting that berberine potentially attenuates brain inflammation via gut regulation.
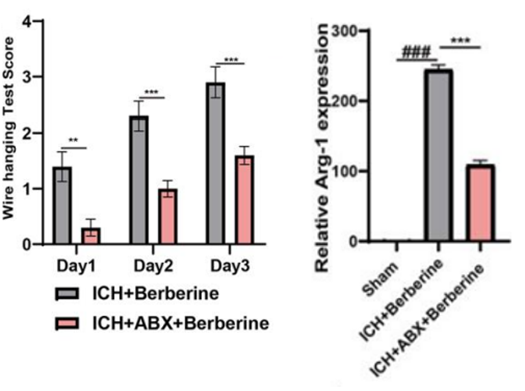
To further evaluate the relationship between berberine, the microbiome, and ICH, the investigators abolished the healthy microbiota in ICH mice and investigated whether these changes affected berberine’s effects on microglia, neuroinflammation, and neurological dysfunction. Chen and colleagues found that eliminating microbiome diversity in ICH mice with a special antibiotic (ABX) reversed all of berberine’s beneficial effects. Even after berberine treatment, ICH mice displayed reduced motor coordination and greater levels of M1 microglia and pro-inflammatory molecules.
After noting the damaging effects of taking away healthy microbes, the investigators were curious to see the potential neuroprotective effects of enhancing microbiome diversity. To do this, the research team conducted fecal matter transplants (FMT) using feces from healthy mice supplemented with berberine. The results showed that ICH mice that received FMT exhibited even better neurological function than berberine-treated mice and presented similar levels of M2 microglia and anti-inflammatory molecules. Collectively, the findings demonstrate that berberine’s neuroprotective effects are likely mediated via the gut microbiome.
Understanding Berberine’s Role in Age-Related Diseases?
While this is the first study to demonstrate that berberine protects against neuroinflammation-induced stroke damage, previous research has shown that berberine also exerts neuroprotection in mice with Alzheimer’s, ameliorating memory deficits and quenching toxic proteins. Importantly, berberine’s ability to cross the blood-brain barrier makes it a primary candidate for aging interventions targeting the brain and nervous system. Interestingly berberine also holds senolytic properties, meaning it can target aged, disease-promoting (senescent) cells that populate nearly all major organs of the body with age. One study found that berberine’s ability to eliminate senescent cells in the heart contributed to delayed cardiac aging. So, while further research is needed to confirm this hypothesis, it’s possible that berberine can promote anti-aging effects by extinguishing senescent cells in multiple organs of the body.
Model: Adult C57 male mice, 8-10 weeks old, with intracerebral hemorrhage (ICH)
Dosage: Berberine 200/mg/kg/d via oral gavage

