Pterostilbene Prevents Diabetes-Induced Memory Loss and Brain Degeneration in New Study
Pterostilbene — found most abundantly in blueberries — prevents cognitive impairments and neurodegeneration while reducing brain and gut inflammation in a mouse model for diabetic cognitive impairment.
Highlights:
- Pterostilbene, but not metformin (anti-diabetes drug) prevents memory impairments and neurodegeneration in a mouse model for diabetic cognitive impairment.
- Treatment with pterostilbene lowers blood glucose levels as effectively as metformin.
- Pterostilbene reduces inflammation in the brain and the gut.
Our bodies can only handle so much sugar, the carbohydrate initially impossible to find in its modern isolated form. However, with the advent of industrialization and world trade, it’s challenging to find a food product without it. Now widely available and often preferred by the masses, sugar, and other processed foods have contributed largely to the increase in diabetes prevalence. Mounting research has shown that diabetes leads to a host of complications, including diabetic cognitive impairment (DCI), the incidence of which is increasing yearly.
Now, researchers from Guangdong University in China show that pterostilbene, rich in Chinese medicines like Dracaena cochinchinensis may prevent many of the most dire consequences of DCI. Published in Phytotherapy Research, Zhang and colleagues show that pterostilbene prevents diabetes-induced cognitive impairment and neurodegeneration, lowers blood glucose levels, and reduces inflammation in the gut and brain, possibly by rebalancing the gut microbiome.
Pterostilbene Prevents Memory Loss and Neurodegeneration while Alleviating Inflammation
To induce diabetes, Zhange and colleagues fed mice a high-fat diet and injected them with a chemotherapy drug called streptozotocin, which damages the insulin-secreting cells of the pancreas. Even after five days of training, these diabetic mice had a hard time finding an escape platform in a pool of water called the Morris water maze (see video to learn more), an indicator of poor learning; establishing these mice as a model for DCI.
When DCI mice were given a low dose (20 mg/kg) of pterostilbene for ten weeks, they did not show the same cognitive impairments as the untreated DCI mice. In fact, the pterostilbene-treated DCI mice found the platform just as well as normal mice. Similar results were shown in DCI mice given a high dose (60 mg/kg) of pterostilbene for ten weeks.
The findings from the Morris water maze test suggest that pterostilbene prevents cognitive impairment in DCI mice. Furthermore, a fourth group of DCI mice that were treated with the anti-diabetes drug metformin (300 mg/kg) displayed similar cognitive impairments to untreated DCI mice, suggesting that metformin does not prevent DCI.
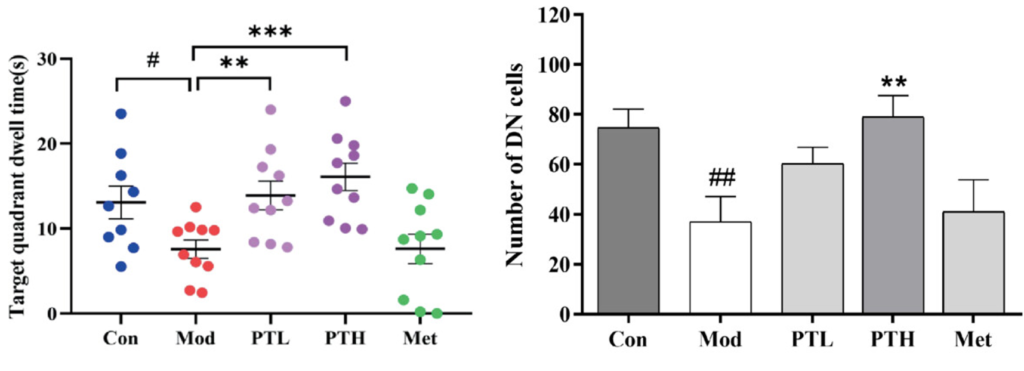
Possibly explaining the cognitive impairments, DCI mice were shown to have increased levels of neurodegenerative markers like neuron death, including dopaminergic neurons – neurons involved in dopamine signaling. β-amyloid accumulation, a marker for Alzheimer’s dementia, was also elevated in DCI mouse brains. Pterostilbene treatment reduced both neurodegeneration and β-amyloid accumulation, suggesting that pterostilbene could prevent DCI by stopping diabetes-induced brain degeneration.
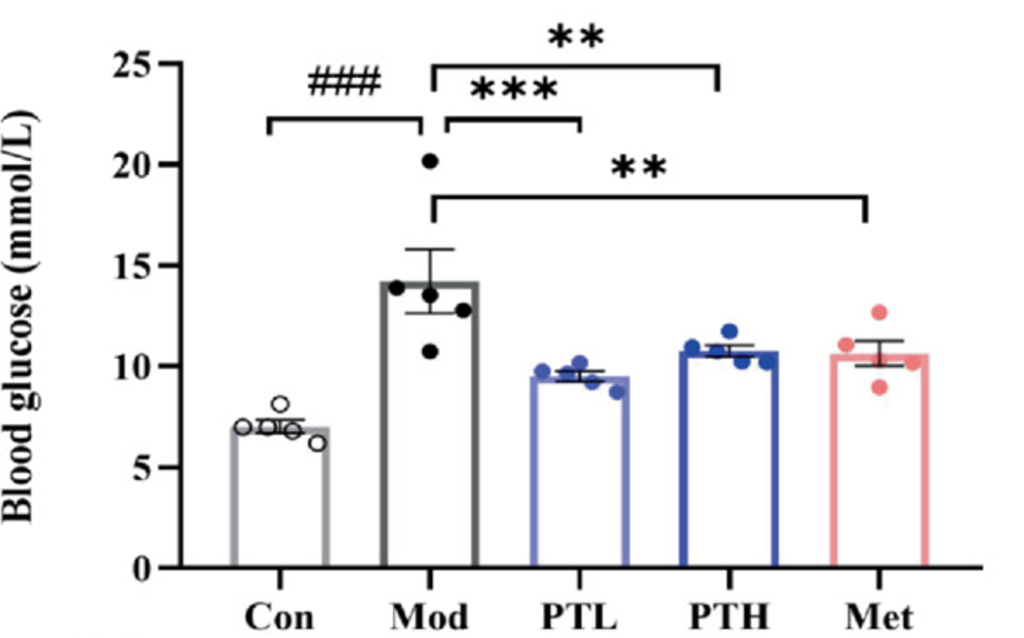
Since insulin allows cells to intake glucose from the bloodstream, a lack of insulin and poor insulin signaling promotes high blood glucose levels. As expected, DCI mice were shown to have high blood glucose levels. Also expected, metformin, a glucose-lowering drug, restored these glucose levels. Furthermore, pterostilbene did the same. These findings suggest that naturally occurring pterostilbene is just as effective as synthetic metformin at lowering glucose levels in DCI mice.
High blood glucose is linked to body-wide inflammation, a condition that over time causes damage to the organs like the brain. It’s this inflammation that may be responsible for diabetes-induced neurodegeneration and cognitive impairment. Since inflammation can affect all organs, Zhang and colleagues measured inflammatory markers from the gut of DCI mice. They found that inflammatory markers like IL-6 were increased in the colon of DCI mice. However, mice treated with pterostilbene or metformin did not show this increase, suggesting that these compounds prevent gut inflammation.
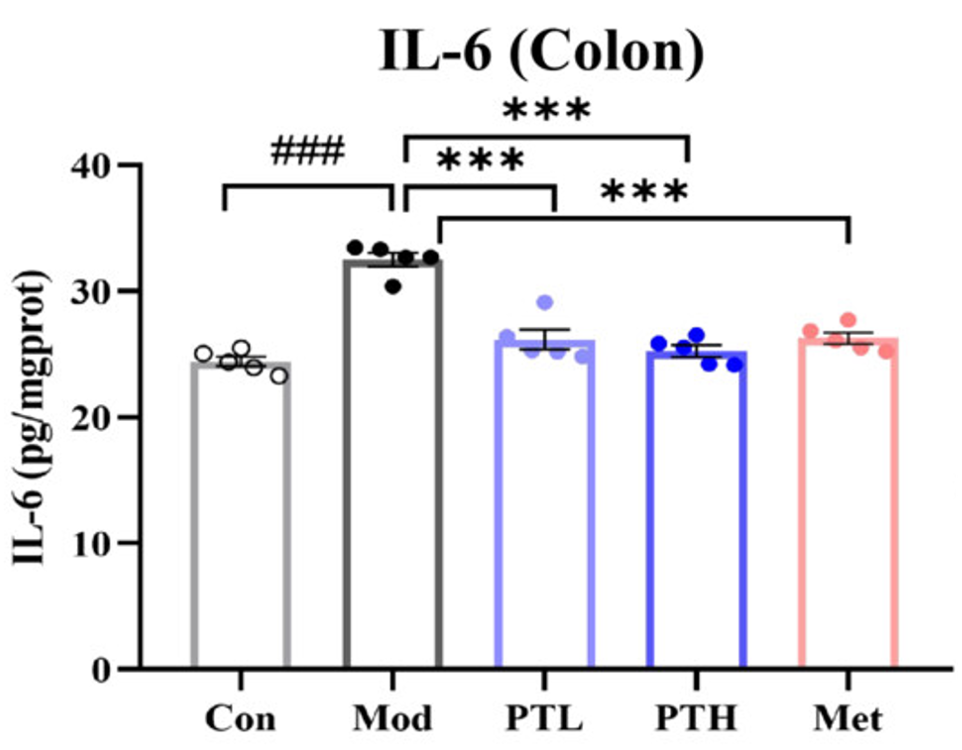
Further experiments showed that the gut wall of DCI mice was leaky, which could allow inflammatory molecules to travel into the bloodstream and reach the brain. Indeed, there was found to be a correlation between gut inflammation and brain inflammation, suggesting that gut inflammation exacerbates the neuroinflammation observed in DCI mice. In turn, pterostilbene treatment was shown to mend the gut wall and alleviate gut inflammation, which further experiments suggested was due to changes in gut bacteria.
Compared to the Popular Anti-Aging Compound Resveratrol, Pterostilbene may be the Better Choice
Overall, the findings of Zhang and colleagues suggest that pterostilbene improves the cognition of DCI mice by preventing brain and gut inflammation via reducing blood glucose levels and promoting the growth of beneficial gut bacteria. Along with the NAD+ booster nicotinamide riboside (NR), pterostilbene is an ingredient in one of Elysium Health’s anti-aging products. This combo has been shown to reduce inflammation in adults with liver disease and slow the progression of ALS.
While more human studies are needed to test pterostilbene alone, it seems like a promising anti-inflammatory. It is also similar to resveratrol, which has been shown to delay heart and muscle aging, improve kidney health, boost memory, and delay reproductive aging in animal models. Furthermore, animal studies have shown that pterostilbene is 60% more bioavailable than resveratrol, potentially exerting similar effects to resveratrol but with lower dosages.
Model: Male C57BL/6 mice fed a high-fat diet and streptozotocin to induce diabetes
Dosage: 60 mg/kg of pterostilbene

