Nicotinamide Riboside Brain NAD+ Elevations Measured for First Time in Healthy Adults
A single dose of 900 mg of nicotinamide riboside (NR) increases brain NAD+ levels in young to middle-aged adults.
Highlights:
- As measured by MRI, brain NAD+ levels were elevated in 9 healthy individuals four hours after ingesting NR.
- Future studies may determine whether raising brain NAD+ levels can combat age-related conditions, such as neurodegeneration and reduced fertility.
The latest research shows that NAD+ levels decline with age in the brain. Furthermore, low brain NAD+ levels may underlie various neurodegenerative and neurological disorders. However, whether brain NAD+ levels can be restored, particularly in healthy adults, has just been illuminated. Remarkably, Ivy League researchers from the University of Pennsylvania (UPenn) show that brain NAD+ levels can be elevated with a single dose of the NAD+ precursor NR.
A total of 10 healthy individuals ranging from 21 to 54 (average: 32) years of age participated in the study. The participants received four MRI (magnetic resonance imaging) brain scans over the study’s course. However, the data from one participant was unusable due to movement issues during the brain scan. Therefore, the results include data from 9 individuals, and there was no control group.
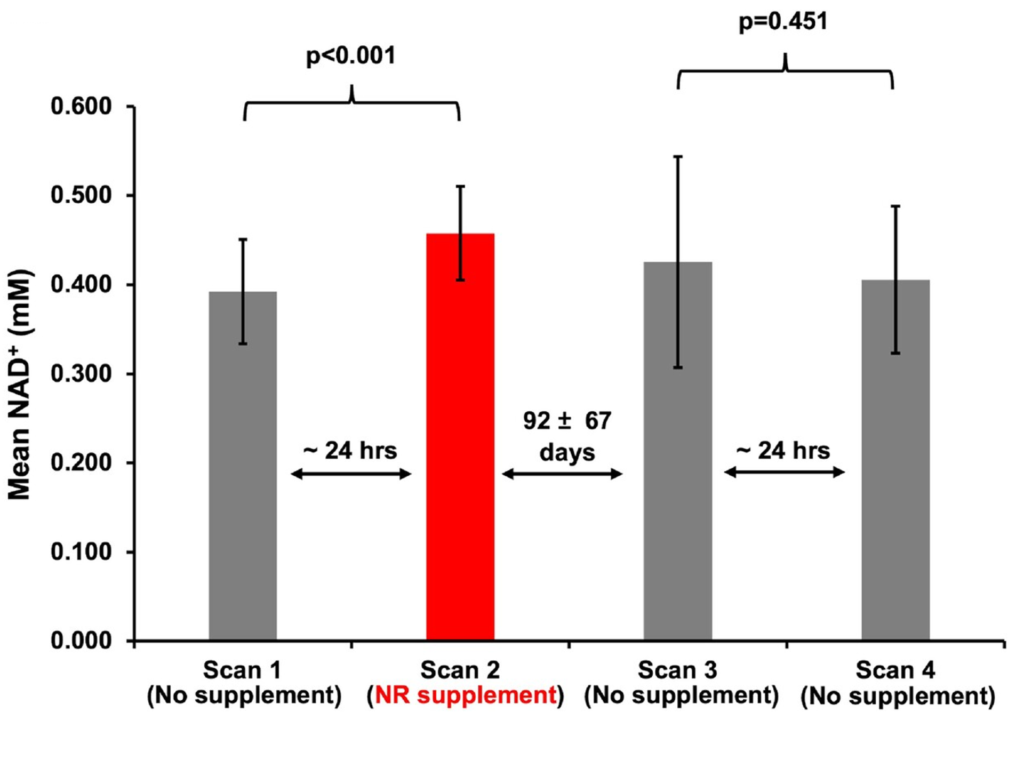
The first brain scan was used to measure baseline NAD+ levels. The day after the first scan, participants took 900 mg of NR early in the morning (5:00 am) and, about four hours later, received a second brain scan. The results of the second scan showed that, relative to the first scan, NAD+ levels increased by 7% to 40%, depending on the individual. On average, NR supplementation led to a 16% increase in brain NAD+ levels. These findings suggest that taking NR orally can increase brain NAD+ levels within four hours.
To test the reliability of these findings, the UPenn researchers performed another set of back-to-back scans but without NR. The time between the second and third scans ranged from 8 days to 5 months, giving enough time for brain NAD+ levels to “reset.” The results showed that, without NR, there were no significant differences in brain NAD+ levels between the third and fourth scans. These findings help to confirm that NR supplementation increases brain NAD+ levels. Furthermore, they suggest that brain NAD+ levels do not significantly fluctuate over the course of two days. More studies will be needed to determine how brain NAD+ levels fluctuate from day to day.
Study Limitations
The authors of the study discuss several limitations to their study design. One is that they did not measure NAD+ levels from the blood or other tissues and organs. Previous studies have shown that taking NAD+ precursors like NR or NMN boosts whole blood, plasma, and circulating immune cell NAD+ levels. However, whether elevations in blood NAD+ levels correlate with elevations in NAD+ levels in other organs, like the brain, remains unknown. Notably, NR does not appear to raise NAD+ levels in the muscle of obese men despite raising blood NAD+ levels.
Another limitation the authors point out is the small number of participants. More participants would increase the reliability of the results. Also, the age range of the participants did not include older adults, who may benefit the most from supplementing with NAD+ precursors. More studies will be needed to determine how NAD+ precursor supplementation affects the brain NAD+ levels of varying populations. Notably, 1000 mg of NR led to elevated brain NAD+ levels and mild clinical improvements in Parkinson’s disease patients.
The authors did not point out the lack of control group. While the main purpose of the study was to show that brain NAD+ levels could be measured in the brain in response to NR supplementation, a control group would increase reliability. Additional studies will be needed to determine the effects of NAD+ precursors on brain NAD+ levels with a larger number of participants that represent the general population and include a group of participants that do not take a supplement to control for confounding variables.
“We demonstrated that a single dose of NR produces a measurable and significant increase in brain NAD+ levels in healthy human volunteers. This pilot study paves the way for future studies that can further assess the effects of NR supplementation protocols on NAD+ concentrations in both healthy subjects and patient populations,” the authors conclude.

