Experimental Cancer Drug Mimics Beneficial Fasting Effects
Treatment with ADI-PEG 20 – an enzyme that degrades the amino acid arginine – improves metabolic health and weight loss in obese mice.
Highlights
- A drug used to treat liver tumors, ADI-PEG 20, improves whole-body metabolism, insulin sensitivity, and fat imbalance in obese mice.
- ADI-PEG 20 mimics these fasting benefits in obese mice by driving arginine turnover and improving liver function.
- The arginine pathway can be manipulated by ADI-PEG 20, which may help treat obesity and related disorders.
Obesity is a multi-organ energy imbalance affecting one of every five people on the planet. While intermittent fasting and caloric restriction are effective therapies against obesity and its complications in mice, intensive lifestyle modifications are rarely sustainable in real-world settings.
Researchers from the Washington University School of Medicine in St. Louis show that a drug typically used to treat liver cancer promotes energy expenditure and insulin sensitivity, as well as reverses various co-morbidities in obese mice. The study, published in Cell Reports Medicine, reveals the unexpected therapeutic utility of a readily available drug called pegylated arginine deiminase (ADI-PEG 20) – which works by affecting the breakdown of the amino acid arginine – in modulating energy metabolism to promote weight loss quickly.
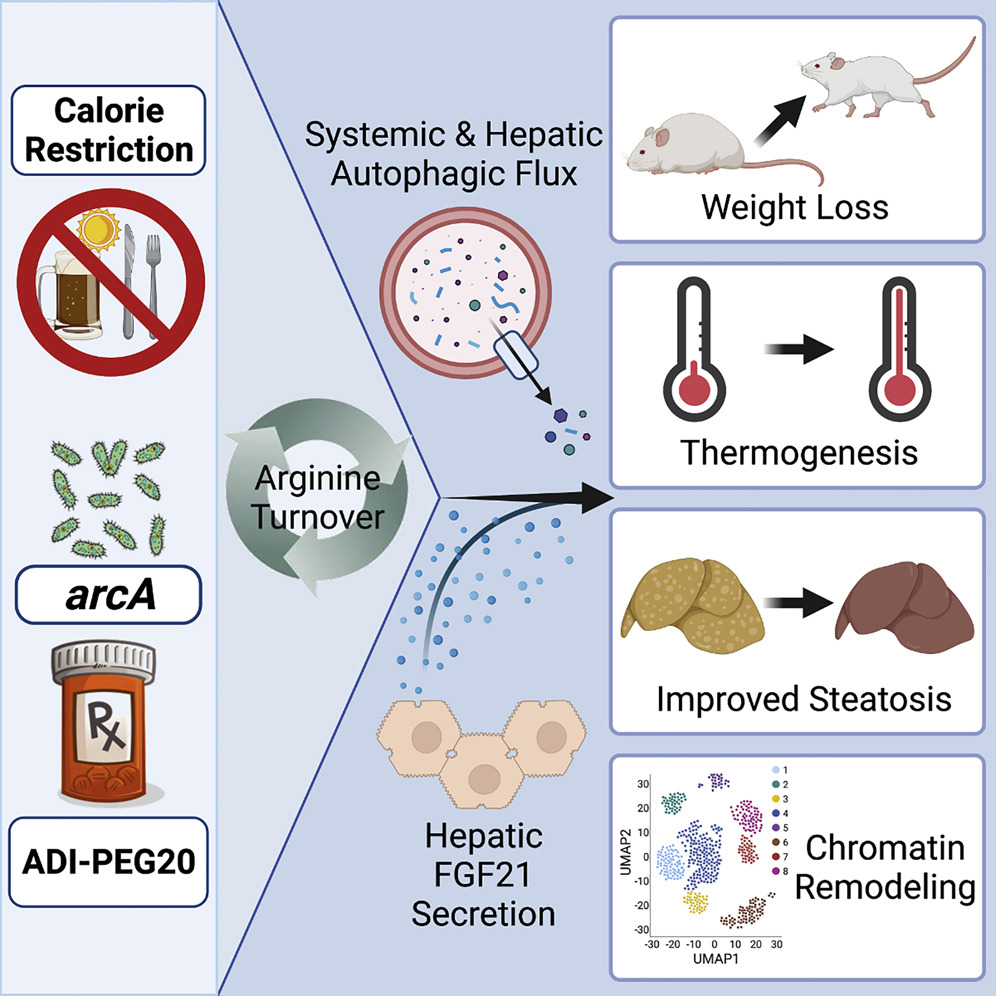
(Zhang et al., 2022 | Cell Reports) ADI-PEG 20 drives arginine turnover and liver function to mimic the benefits of fasting. Arginine deprivation induces adaptive liver (hepatic) fasting-like responses, resulting in weight loss, thermogenesis, and improved fatty liver (steatosis). The readily available pharmacotherapy ADI-PEG 20 leverages this pathway.
ADI-PEG 20 improves whole-body metabolism.
Zhang and colleagues gave diabetic mice ADI-PEG 20 injections weekly for five weeks before metabolic tests and tissue analysis. Compared to untreated diabetic mice, ADI-PEG 20 lowered weight gain, decreased fat mass, and raised lean mass. Notably, the total daily food consumption of the mice dramatically declined after treatment with ADI-PEG 20. When the researchers analyzed the changes in body weight and food intake side by side, they observed that body weight decreased before there were noticeable changes in food consumption. These beneficial changes in body composition occurred without the mice changing their breathing capacity and movement frequency.
Zhang and colleagues showed that processes other than food consumption are more likely to be at the root of ADI-PEG 20’s immediate therapeutic effects on body mass. By analyzing the liver’s metabolic profile, Zhang and colleagues showed that ADI-PEG 20 therapy had other advantages, such as considerably decreasing cholesterol and non-essential fatty acid levels in the liver. These metabolic changes were confirmed by the proportion of fatty (steatotic) liver, which decreased substantially in ADI-PEG 20-treated animals. These findings reveal that a commonly accessible medicine that produces arginine deficiency is enough to trigger an adaptive liver cell fasting-like responses.
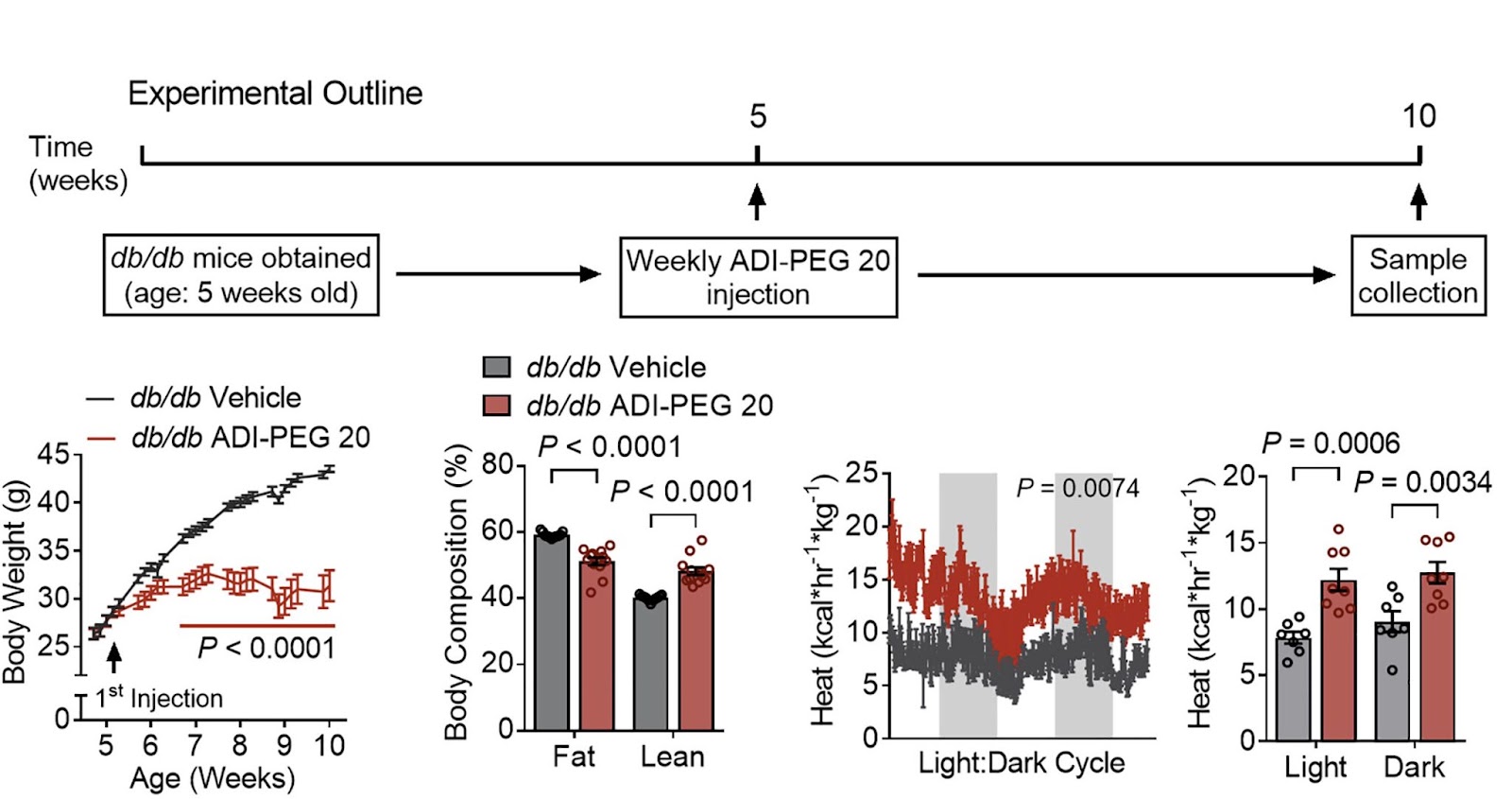
(Zhang et al., 2022 | Cell Reports) ADI-PEG 20 treatment improves whole-body metabolism and heat production. (Top) Five-week-old male diabetic mice were randomly grouped and treated with saline (control) or ADI-PEG 20. (Bottom) ADI-PEG 20 led to improvements in body weight (left), whole-body fat and lean mass percentage of composition (center left), and energy expenditure during light and dark cycles (right.
Zhang and colleagues also found that ADI-PEG 20 alters the accessibility to the genome, also known as epigenetic changes, in liver cells in a manner that corroborates improved liver metabolism upon systemic arginine deprivation. These liver cell epigenetic changes in conjunction with ADI-PEG 20’s metabolic effects would extend the effectiveness of arginine depletion beyond the drug’s dose. The well-known epigenetic and long-lasting impact of intermittent fasting and calorie restriction on host metabolism provide a precedent for this finding.
“Giving this drug seems to mimic some of the metabolic and therapeutic effects of fasting,” said senior author Brian DeBosch, MD, Ph.D., an associate professor of pediatrics. “I was surprised by how large the effect was. In the mice prone to weight gain, the group that received the drug ended up weighing about 25% less than the mice that didn’t get the drug. And in the mice on the high-fat, high-sugar diet, we saw similar weight loss from the drug. Also, we don’t think that the preponderance of the drug’s metabolic benefits are from changes in body weight. In fact, for several outcome measures, the metabolic changes preceded significant changes in weight.”
Proceeding with caution
L-arginine is a semi-essential amino acid and is one of the most versatile amino acids with multiple competing metabolic fates in the liver. This raises the possibility that long-term perturbation of arginine could negatively impact other aspects of metabolic function.. In the current study, mice were treated with ADI-PEG 20 for up to 5 weeks without apparent adverse effects.
Importantly, two human trials treated patients with ADI-PEG 20 between 8 and 41 weeks. These patients were evaluated for toxicities induced by treatment with ADI-PEG 20, which ended up being on the lower end. In a more recent clinical trial involving patients with advanced liver cancer (hepatocellular carcinoma) and other gastrointestinal malignancies, 24 weeks of arginine depletion was maintained in patients with no major side effects other than reductions in blood cell types. All of the situations were successfully settled and managed.
Furthermore, human studies have shown that fast- and long-lasting arginine depletion is safe up to 18 weeks after initial dosage. A phase 3 experiment is underway to determine ADI-PEG 20 durability for 103 weeks after starting treatment (NCT03449901). There is no evidence for metabolic consequences of chronic arginine deficiency.
Putting the current study into context with the clinical data, Zhang and colleagues suggest that perhaps short-term arginine-targeting treatment has therapeutic benefit, regardless of its persistence. This may address an unmet need in the treatment of obesity, whereby rapid weight loss before bariatric surgery improves surgical results.
“Many patients with obesity who are considering bariatric surgery must first lose some weight to make the procedure safer,” said senior author Brian DeBosch, MD, Ph.D., an associate professor of pediatrics. “It can be difficult for such patients to lose up to 10% of their body weight before the surgery. This type of therapy could potentially serve as a bridge to help patients lose weight before bariatric surgery, to reduce the risk of complications during and after the procedure.”