Anti-Aging Compound Curcumin Outperforms Chemotherapy in Cancer Model: Kyoto University
Japanese scientists develop a synthetic form of curcumin — known for its anti-aging and anti-inflammatory properties — that shrinks tumors in a mouse model for chemotherapy-resistant bone marrow cancer (multiple myeloma).
Highlights:
- A drug called TBP1901 is converted to curcumin in bone marrow and is more biologically active than curcumin.
- TBP1901 shows significant anti-tumor effects in a mouse model for multiple myeloma – an age-related bone marrow cancer.
- Cancer growth in vitro (in a dish) is inhibited more by curcumin than TBP1901.
Turmeric – a major source of curcumin – has been used in Asian cultures as a spice and cure-all for millennia. Recent studies have come forward that in addition to its anti-aging and anti-inflammatory properties, it may also have anti-tumor properties. However, the bioavailability — ability to be used in the body — of curcumin may not be ideal. Thus, to help enhance its known positive benefits, researchers out of Kyoto University in Japan modified curcumin into a prodrug – an inactive compound that requires metabolism by the body before becoming biologically active.
As published in the European Journal of Pharmacology, Abe and colleagues focused on testing the effects of the curcumin prodrug TBP1901. They found that TBP1901 metabolized to its active form most greatly in bone marrow, leading them to use the drug on a multiple myeloma mouse model — a model for age-related bone marrow cancer. The researchers found that TBP1901 had significant anti-tumor effects, effectively shrinking tumors in mice. However, TBP1901 did not have strong effects in preventing cancer cell growth in a dish (in vitro). Still, regular curcumin had anti-tumor effects in vitro.
TBP1901 has Anti-tumor Effects
After developing the curcumin prodrug TBP1901, Abe and colleagues found that it was converted to curcumin by a protein called β-glucuronidase and achieves higher blood curcumin levels than oral versions. The greatest β-glucuronidase activity and conversion to curcumin were found in the bone marrow of both monkeys and mice upon injection of TBP1901.
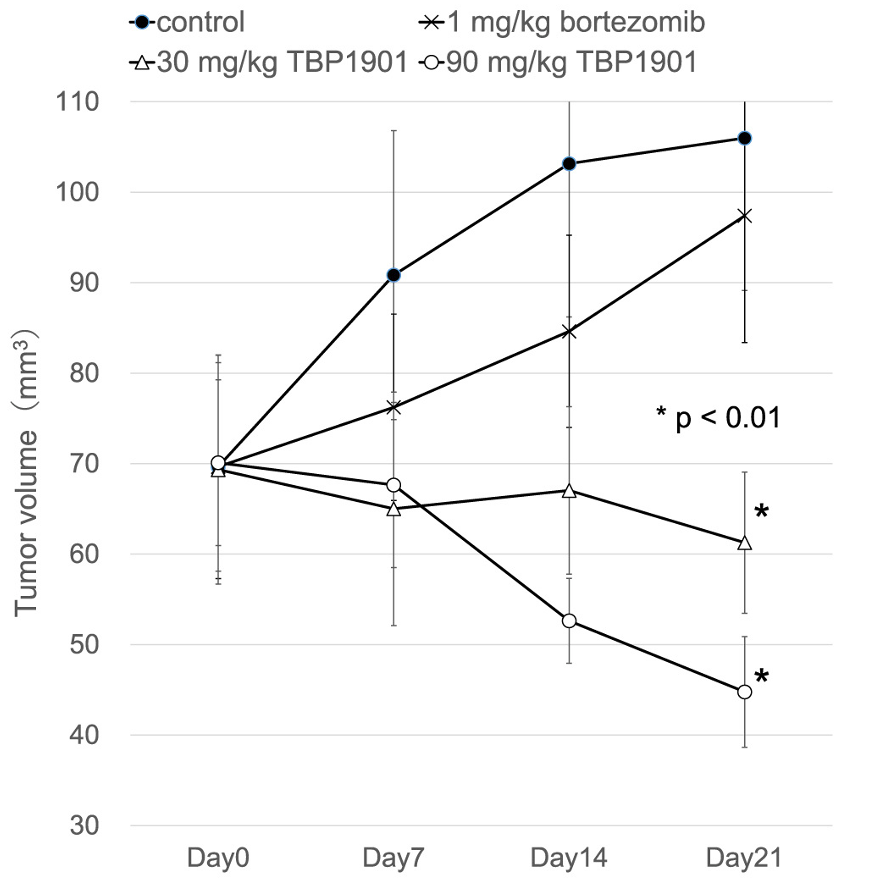
Because of the high bone marrow conversion rates, the researchers looked at the effects of TBP1901 on bone marrow cancer, specifically multiple myeloma. To model this cancer, chemotherapy-resistant myeloma cells were transplanted under the skin of mice with compromised immune systems. Injecting TBP1901 into these mice significantly decreased tumor volume in a dose-dependent manner, even when compared to the chemotherapy drug bortezomib.
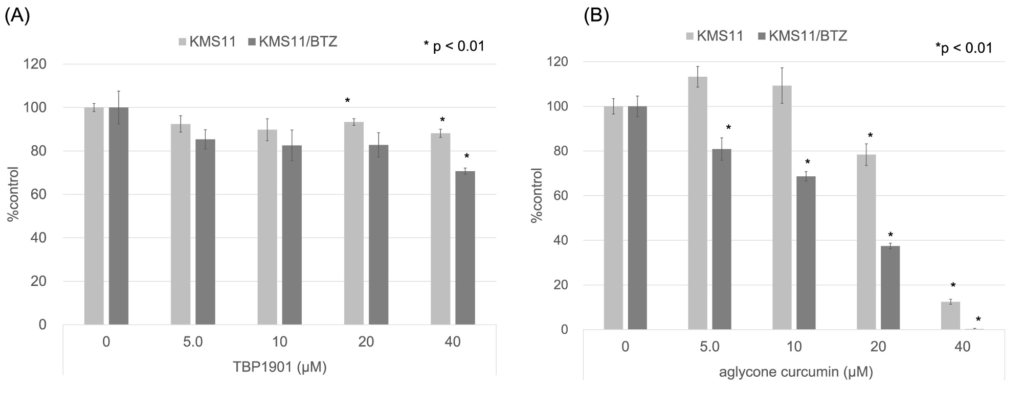
Abe and colleagues also compared the effects of multiple myeloma cancer cell growth between TBP1901 and curcumin in vitro. They found that, despite the anti-tumor effects in animals, TBP1901 did not affect cell growth and division (proliferation), except at high doses. In contrast, curcumin (aglycone curcumin) decreased cell growth and division in a dose-dependent manner with effects at even low doses. It is unclear why TBP1901 had less of an effect than curcumin, but this is likely due to a lack of β-glucuronidase in the cancer cell culture.
TBP1901 versus Curcumin Against Age-related Diseases
Multiple studies have indicated that curcumin’s anti-oxidant and anti-inflammatory properties have made it a useful treatment for a myriad of age-related diseases, including cardiovascular disease, numerous cancer types, and diabetes. But outside of age-related diseases, curcumin has also shown promise in just maintaining health as we age. Studies done in roundworms have shown that curcumin can actually prolong lifespan, while other studies done in mice have shown that curcumin can help maintain our cognitive health as we age.
The evidence of curcumin’s potential as an anti-aging and anti-inflammatory compound is increasing. However, its bioavailability is still a concern. Often when taken orally, a large percentage of the curcumin gets broken down into inactive compounds. In this study, Abe and colleagues have used targeted liposomes with a prodrug form, TBP1901, to get the curcumin where it needs to go, and it seems to have been more effective at treating age-related bone marrow cancer than conventional curcumin compounds.
However, whether TBP1901, or any other modified, more bioavailable curcumin forms, is better in terms of anti-aging has yet to be seen. More research, including clinical trials focusing on TBP1901’s anti-aging effects, is warranted before determining whether TBP1901 is a better version of curcumin, although the evidence points towards that being the case.
Model: C57BL/6J mice
Dosage: 30 to 90 mg/kg TBP1901 injected intravenously

